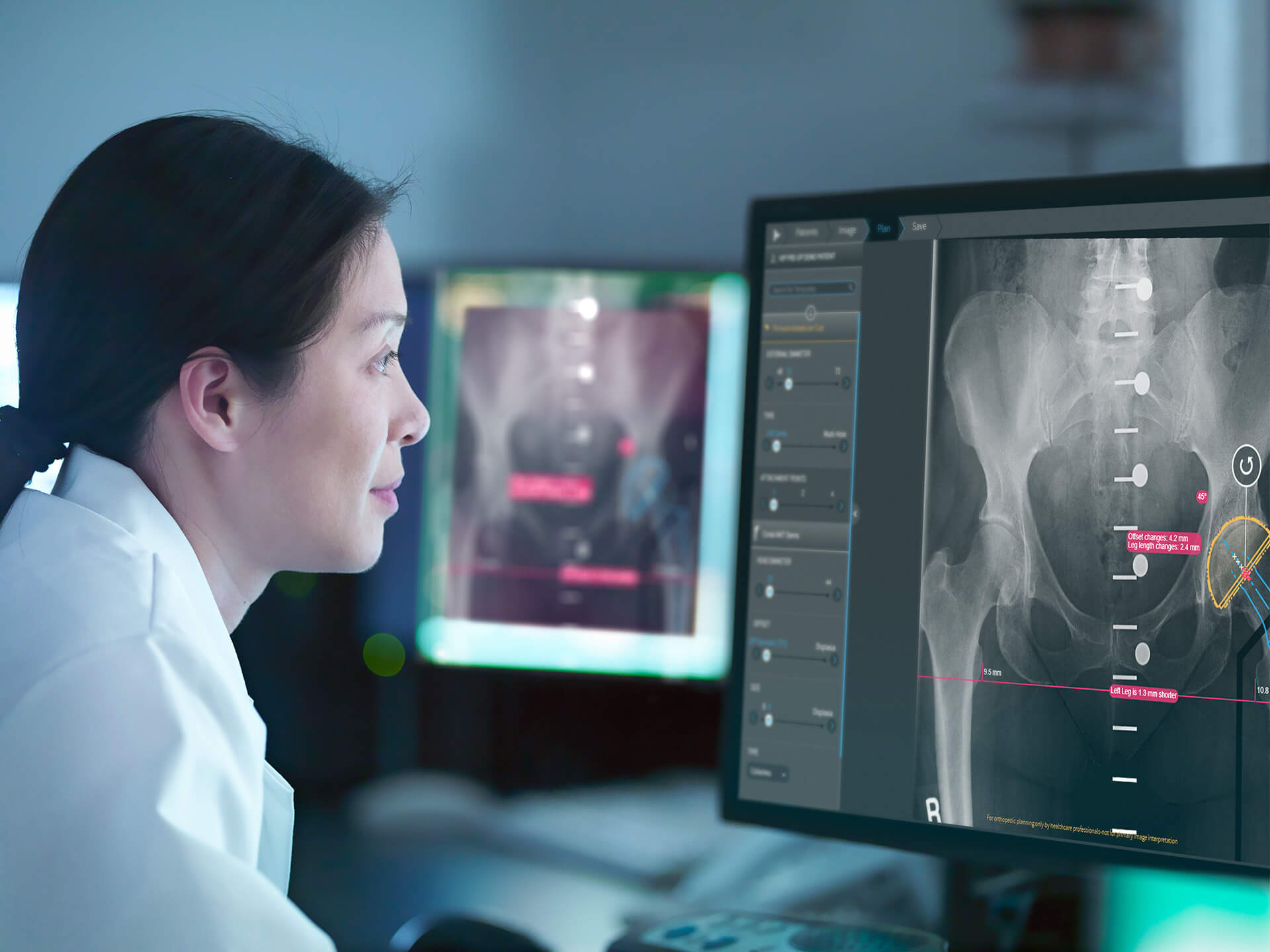
TL,DR: Using a complete and standardized workflow for orthopedic surgery preoperative planning can support the best possible treatment outcomes for patients. The 7 steps below outline a preoperative planning workflow designed to both streamline the process and identify potential gaps in standard planning routines.
Over the last few decades, orthopedic preoperative planning has been widely adopted as a result of advancements in technology and the integration of digital tools. But, when looking at day-to-day planning routines, what are the basic rules of thumb for creating a preoperative plan that make a difference?
1. Carefully review and confirm imaging
When it comes to preoperative planning, accurate images are everything.
All images received from radiographers should:
Be captured from the correct viewing angle – not rotated
Be in full size – not cropped
Have the right contrast – not too bright or too dark
2. Calibrate for accurate digital templating
Accurate calibration is a major step towards achieving precision in preoperative planning. Using calibration markers facilitates accurate digital templating [1] and helps reduce magnification errors caused by the patient size and position.
Whether you’re taking anteroposterior (AP) pelvic images or preparing for knee, upper limb or foot & ankle procedures, for the most accurate preoperative planning process, the right type of calibration device is needed.
For AP pelvic X-Ray images, it is recommended to use a double-marker calibration tool, which is automatically recognized by preoperative planning software. For example, in the clinical study, A novel method of accurately calculating the radiological magnification of the hip, the double marker calibration method was shown to be superior to conventional, single-ball markers [2].
For all other procedures, it is recommended to use a single marker device positioned at the level of the bone. This type of device is also automatically recognized by the preoperative planning software.
Read more about orthopedic calibration here.
3. Perform anatomical assessments
Before starting to template the image with the right implants, start by assessing the patient’s anatomy, and check for specific measurements that may inform the right surgical decisions [3].
Preoperative planning software provides enhanced tools to assess the patient’s anatomy for every case, so the preoperative planning process can begin after collecting valuable data on the patient’s condition.
For example, check the Reimers migration percentage or the hip center of rotation, analyze the limb alignment or determine the resection lines.
4. Measure twice, cut once
Accuracy is a key factor for the success of a surgery, but accuracy during surgery starts way before the first incision is even made.
According to a range of clinical studies, accurate templating and sizing of implants in orthopedic surgeries can reduce the risk of complications [4] and the procedure’s duration [5], [6]. Ultimately, it saves valuable time in the O.R. by enabling surgeons to determine the right implant size ahead of time.
As part of the preoperative planning process, be sure to collect all the measurements needed, confirm template sizes and simulate the outcomes of the hip reduction or the knee alignment in advance.
5. Involve the patient
Surgery can be a stressful experience for patients, and a picture is worth a thousand words. Use your planned case to provide patients with details about the upcoming procedure and show them the expected results.
6. Bring all the information together
After successfully planning the case, this is the right time to organize all the relevant pieces of information needed to prepare for the surgery.
Generate pre-surgical reports including patient details and images, implant information, measurements taken and comments.
7. Measure your success
Although it might seem like it, the orthopedic planning process doesn’t end immediately after the surgery is completed. To truly determine if your preoperative plan was accurate enough, the postoperative verification stage is critical.
Leverage the data you collected and connect it from preoperative planning to postoperative analysis to create an insightful treatment assessment for you, your surgical team and your patient.
For example, use postoperative anatomical analysis tools to compare your planned case with the actual outcomes of the surgery, or assess the implant condition and patient satisfaction over time. Taking the time to carefully review the process and the insights generated from the preoperative and postoperative tools and applying them to future plans supports increasingly streamlined surgeries in the future.
When it comes to the complete cycle of orthopedic planning, these 7 steps can standardize success for orthopedic surgeons.
1. Baxter, J., Barlow, T., Karthikeyan, S., & Mayo, D. K. (2012). The Accuracy of Automatic Calibration of Digital Pelvic Radiographs Using two Different Scale Markers: A Comparative Study. HIP International, 22(1), 82-89.
2. King et al., A novel method of accurately calculating the radiological magnification of the hip, J Bone Joint Surg Br. 2009 Sep;91(9):1217-22
3. Wek C, Chowdhury P, Smith C, Kokkinakis M. Is the Gothic Arch a reliable radiographic landmark for migration percentage in children with cerebral palsy? J Child Orthop. 2020 Oct 1;14(5):397-404.
4. Amro Alnahhal, Nayef Aslam-Pervez and Hassaan Q. Sheikh (2019) Templating Hip Arthroplasty
5. Atesok K, Galos D, Jazrawi LM et al. (2015) Preoperative Planning in Orthopaedic Surgery. Current Practice and Evolving Applications. Bull Hosp Jt Dis (2013) 73:257–26
6. Hsu AR, Gross CE, Bhatia S et al. (2012) Template-directed instrumentation in total knee arthroplasty: cost savings analysis. Orthopedics 35:e1596-600.