Webinar
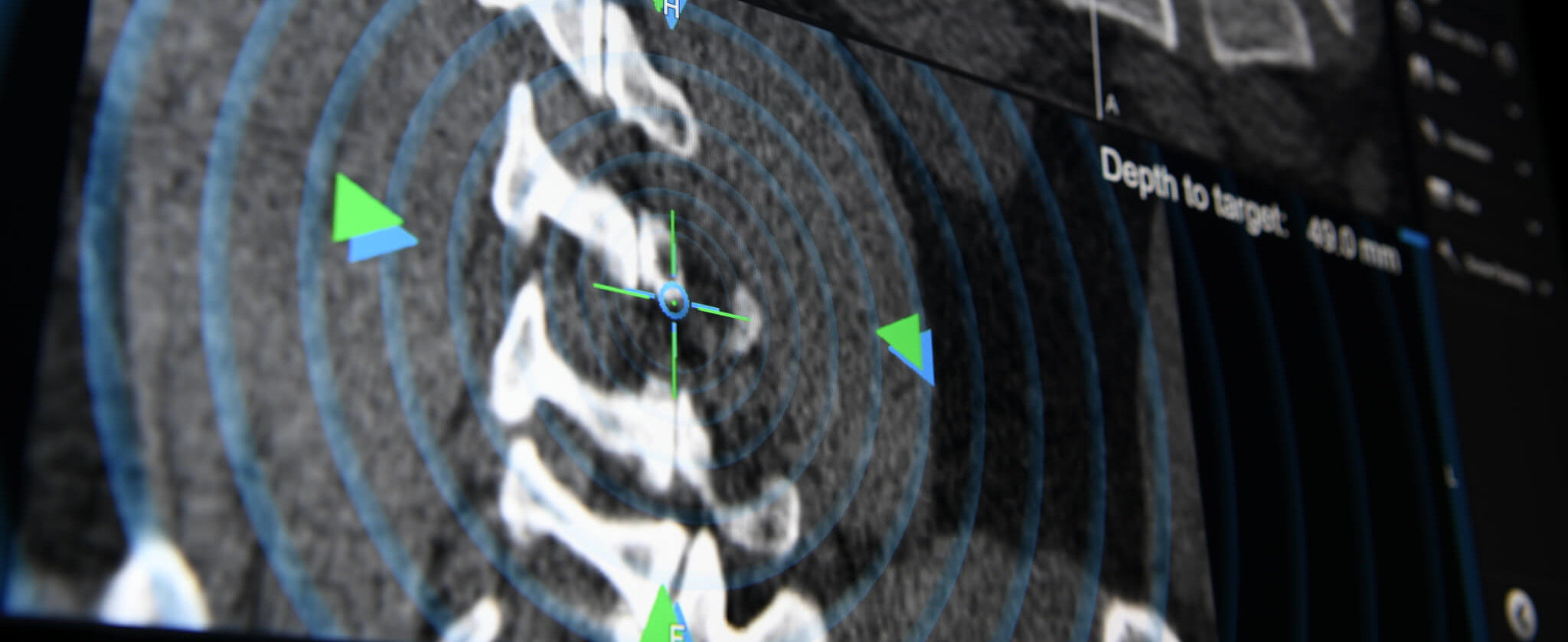
Spine Navigation and Navigated Drill-Guide Technique: Accuracy where it matters without any compromise
Jun 10, 2021
Descrição
Brainlab invites you to a live webinar: “Spine Navigation and Navigated Drill-Guide Technique: Accuracy where it matters without any compromise” on June 10th at 5:00 PM (CET) hosted by Prof. Krieg on his successful use of spine navigation and its different application using navigated drill guides and image registration.
This webinar will cover:
The use of navigated drill guides in combination with various image registration methods
Detailed case reports including cervical, MIS tumor and long construct
Pitfalls of navigation and how to avoid typical errors to gain the best possible surgical result
We look forward to meeting you online!
Language | English
In case you can’t join the webinar, it will be recorded and shared afterward.
Participation is free of charge.
The views, information and opinions expressed during this presentation are the speaker’s own and do not necessarily represent those of Brainlab.

Sandro Krieg, Dr. M., MBA
Professor de Neurocirurgia, Diretor médico da Clínica de Neurocirurgia da Clínica Universitária de Heidelberg