Webinar
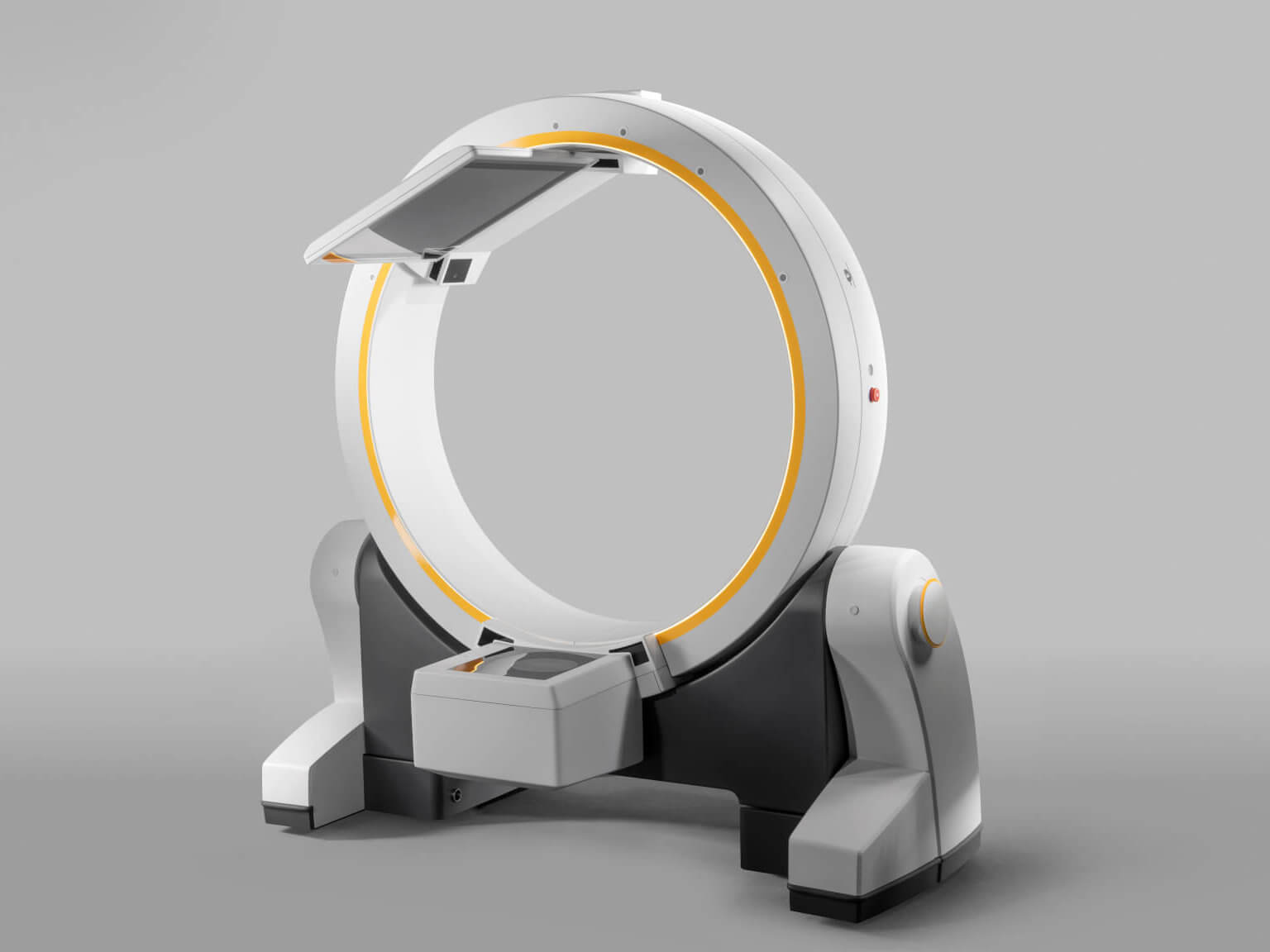
Expanding my Craniomaxillofacial intraoperative imaging experience with Loop-X, a mobile imaging robot
Mar 16, 2021
Beschreibung
Brainlab invites you to join our live webinar, “Expanding my Craniomaxillofacial intraoperative imaging experience with Loop-X, a mobile imaging robot”, on March 16, 2021 at 4:00 PM CET presented by Simon Enzinger, MD, DMD, Managing Senior Physician at the University Clinic for Oral and Maxillofacial Surgery in Salzburg, Austria
We look forward to meeting you online!
Language | English
In case you can not join the webinar, it will be recorded and shared afterward.
Participation is free of charge.
The views, information and opinions expressed within this presentation are from the speakers and do not necessarily represent those of Brainlab.
Sprecher:in:

Simon Enzinger, MD, DMD
University Hospital Salzburg, Austria
Moderator:in:

Jana Guggenberger, Director Product Management & Marketing Spinal/CMF Planning/Navigation
Weitere Webinare anzeigen
Jetzt anmelden