Read the transcript below
“I’m excited about the opportunity to present my vision to you this afternoon. Digital health represents a tremendous opportunity for growing closer in Europe, and staying healthy together. Let’s now focus on leveraging artificial intelligence (AI) and digital technologies for inpatients.”
Brainlab President & CEO Stefan Vilsmeier outlines his vision for 2021 and beyond: “We can digitalize surgery by leveraging artificial intelligence and digital technologies, allowing access to more consistent treatments for every patient and the dissemination of knowledge and best practice.” Watch the video below or skim the transcript.
Read the transcript below
“I’m excited about the opportunity to present my vision to you this afternoon. Digital health represents a tremendous opportunity for growing closer in Europe, and staying healthy together. Let’s now focus on leveraging artificial intelligence (AI) and digital technologies for inpatients.”
Digitizing surgery
“The core of a hospital is surgery. The operating room is the number one value driver, but also the biggest efficiency leak, due to many analog processes. In order to provide access to better and more consistent treatments for every patient, to leverage AI, and to disseminate knowledge and best practice, we must digitize surgery. I now want to provide you with insights into state-of-the-art in surgery today.”
Connecting data to create a “Google Maps for the human body”
“The biggest opportunity for AI is the connection of data between different domains, like Google Maps connecting the actual digital map with GPS coordinates, leveraging a powerful statistical database, with layers for topography, traffic flows and public transportation. The augmented Street View links to this database to create the unique ecosystem that makes Google Maps so powerful. So, how can we create a kind of Google Maps for the human body?”
“I start by using this Digital O.R. system to aggregate and correlate data from different diagnostic sources, creating a digital twin of the patient. I use this AI-based brush tool to define the tumor, and by then moving to get a 3D view that provides me access to the different layers of anatomy that I can peel away, like the different layers of an onion, making the anatomy computer processable.”
“This is possible through a universal anatomical model that is based on a massive database that contains variability, relational knowledge, and clinical properties of thousands of structures. When I move further here, I see the so-called fiber tracks, the telephone wires of the human brain. In neurosurgery, I can use them to access the tumor and avoid those structures, however, they can be used based on AI algorithm to simulate the spread of tumor cells in the brain.”
“Let’s now move towards the surgical equivalent of a GPS system. We will use this camera to track the position of a surgical instrument in real time. As we move the pointer over the surface of the skull, you can see in real time the position of my instrument, and all the structures underneath, and how I can safely access my tumor past my critical structures. By tracking an instrument, I digitize the path to my tumor for this patient, but by doing that over multiple patients, I can aggregate powerful data and knowledge.”
“Now, let’s add video. Neurosurgeons rely on microscopes to resect tumors, and of course, a microscope only reveals the surface of the anatomy. However, by now adding augmentation, you can see the structures underneath, such as the tumor and how it extends beyond what is visible, but also the fibers and the structures that wrap around the tumor.”
“You have just seen how the microscope moved robotically. And in fact, there is a growing number of solutions that are robotic and help assist surgery, such as these type of arms that I can use to align to a particular trajectory. Then I can automatically get the perfect access to my tumor, or those supported imaging devices that can take additional images during surgery update my anatomical model. So you can imagine how those robotic solutions create a wealth of additional data, and therefore a tremendous opportunity for AI.”
“Going back to the example of Google Maps, it is the linking of these domains that creates a powerful ecosystem. We need to aggregate and share data across multiple patients to unlock better treatments of life-threatening diseases, or even enable cures. Right now, a lot of treatment concepts are overly simplistic. They’re more or less based on a one-size-fits-all approach, with very little customization. For example, despite 50 years of research and 3000 papers published on the treatment of brain metastases, we’ll still use either 23, 18, or 15 Gy on those. Why not 19.3 Gy? We need to analyze large amounts of very carefully validated and recorded treatment results to get better answers and achieve personalized treatments for every patient.”
Moving towards value-based care
“For inpatients, it is important to move from paying for a specific procedure independent from the patient benefit to value-based care. We need to capture and evaluate the entire treatment process. This will provide all citizens with better care at lower cost.”
“There are three areas we need to focus on: We need better data, we need to share this data, and we need to become better at using the data and the products derived from that data.”
Generating better health data
“How do we get better data? The typical hospital information system has been built over decades with billing and administrative needs in mind, not around the level of detail necessary and meaningful from a clinical perspective. However, innovation will gravitate to where the best data is available.”
Set Fast Healthcare Interoperability Resources as the standard
“One of our core problems that we need to address is the standardization of data, data semantics, and interfaces. For decades, the healthcare system has struggled to connect system A to system B, even within the same hospital. Now we want to connect data across hospitals, apps, developers, and domains. Much of the world has begun to rely on the standard of Fast Healthcare Interoperability Resources (FHIR), which is based on an internet technology widely used in industries outside of healthcare. It is time for us to do so as well. The HL7 FHIR standard defines how healthcare information can be exchanged between different computer systems regardless of how it is stored in these systems. FHIR significantly lowers the barrier of entry for new software developers to support healthcare needs.”
Promote structured data
“Everybody talks about the need for structured data. The clinical notes in the average EHR won’t get us far. They’re not sufficient in terms of machine readability and quality. We need to capture data primarily through structured workflows, following established clinical guidelines. This ensures conformity and completeness of documentation, for example, radiology reports or tumor board meeting documentation. Moreover, it will provide objective data driving AI, such as detailed radiomics, and enable effective longitudinal studies of degenerative diseases or cancer. We need to move away from unstructured notes, and provide patients and caregivers across Europe with an objective assessment of disease severity or classification, and therapy response.”
Use Patient Reported Outcome Measures
“One of the very successful steps the U.S. has taken towards value-based care was the promotion of incorporating patient reported outcome measures (PROMs) into the care cycle. In essence, the patient would receive a text message or email asking to complete a detailed survey to assess their functional performance and quality of life after their hospital stay. This enables remote patient monitoring to detect a potential problem, and to alert the care team to take appropriate action. PROMs also allow comparison of patient outcomes across different therapy methods, healthcare facilities, and therapeutics in much greater detail, and, very importantly, from an unbiased patient perspective. In order to ensure all patients in Europe receive the same level of care, and for the EU to become competitive in AI, we need to broadly adopt PROMs.”
Extract data from images and plans
“We now want to focus on the opportunity of image data. I previously introduced the concept of structured diagnostic and video data using my Google Maps analogy. For any cancer registry, we need to capture not only the detailed assessment of volumetric treatment response, but also the correlation of relevant treatment parameters along the patient pathway, such as the distribution of radiation dose in relation to complications. With a large-scale effort, Europe can lead the world in volumetric tumor data, attracting leading clinical and industrial researchers, so we can beat cancer together.”
Sharing health data
“Neither American data capitalism nor Chinese data socialism are consistent with our European values. Together, we can build what I call a social data economy. That will allow for patient-centric, empowering, discrimination-free participation in better health care for every citizen in Europe. The European Health Data Space will serve as the legal and regulatory framework to achieve this. Industry needs to actively participate in collaboratively creating a technical infrastructure on the foundation of safety, privacy, and transparency. An infrastructure that all patients can trust.”
“With the GDPR, Europe has data protection rules that have become a role model for the world. Let’s build a framework together specifically for healthcare, that can achieve the same, because without a data strategy, there will be no AI strategy. Here is what it will take.”
Standardize universal patient consent
“If our goal is a patient-centric concept, we need to start with capturing the patient’s will relative to healthcare data in a meaningful granularity. Such consent should be standardized, following a broad public debate, and it should be universally applicable to at least all inpatient data.”
“If I put myself in the shoes of a patient, and probably at some point, I will be in the role of a patient myself, I prefer to record my intent independent of the emotional stress of a specific emergency. Consent needs to include specifics for using select types of data, possibly for specific clinical fields, and clearly defined groups of potential users. A digital version could move from coarse to fine, allowing me to customize step-by-step the settings and the granularity I want. It is important that we specifically separate between clinic, science, and industry. For example, a patient may consent to having data shared just for a specific disease field, with just the manufacturer of the products involved with his or her treatment. Standardizing such a patient consent could be a crucial cornerstone towards the European Health Data Space.”
Establish an industry-wide code of conduct
“In Europe, society is generally cautious about how digital data is being used and shared with industry, which is deeply rooted in our value system. To address this, we need a clear and consistent set of rules for all players: a code of conduct. The code of conduct should be designed to execute the previously discussed universal patient consent in a trustworthy way. I advocate a compulsory requirement of licensing data within a circle of authorized recipients per the consent at reasonable terms. This will promote data-driven business models based on generating incremental value of data, and will sanction models just based on “taking over the toll booth”.”
Sanction closed turnkey solutions
“Reimbursement in healthcare has created an incentive for mostly large medtech companies to lock in a complete value chain around a specific treatment, by orchestrating several data-driven products around an implant, for example. The results are overpriced and incompatible monolithic island solutions that are resulting in data silos. This cripples competition and market access for small companies, resulting in more expensive and less innovative treatments. All industry players should be required to design and offer open, interoperable systems that should encode semantics, to the extent possible, on FHIR, following applicable implementation guidelines, and fully disclosed data models. Connecting new solutions should require no project effort or costs for healthcare providers. All of this should be a prerequisite to participate in public tenders.”
Separate personalized data and healthcare data
“Companies processing search engine queries, GPS data, or natural language are in a privileged position for profiling citizens. However, I feel very uncomfortable with the same company processing healthcare data. The GDPR calls for “privacy by design”. Based on this principle, I propose an organizational and legal separation between these types of data processing companies. This would require Amazon, Google and Microsoft to adapt their European health ambitions to European values, and establish organizational, legal and technical walls between consumer data and healthcare data. Such initiative would open up fair opportunities for hundreds of companies to compete on the merits of their innovation, and in line with our European values.”
Develop a distributed data sharing infrastructure
“A big part of the discussion on shared data circles around central data repositories, and in fact, big data registries provide valuable insight. At the same time, there are hundreds of smaller multicenter clinical trials and specialized data hubs that are critical for keeping innovation processes agile, and Europe competitive. I propose to implement a hybrid structure for the European Health Data Space, that combines centralized and decentralized data clusters, using trust centers of different scope or reach, that can synchronize data as needed, and in line with the patient consent provided. Such a federal model is more in line with the structure of Europe, and allows synchronization of multiple national registries without slowing anybody down.”
Using health data to its fullest
“We also need to remove barriers for using data. We need to harmonize the national interpretation of GDPR across Europe, and use the opportunities of the regulation for the benefit of all patients. Not using this data is killing people at scale.”
Provide broad access for federated learning
“I dream of a framework that makes Europe the leading hub for AI developers in healthcare, with safe and privacy-preserving access to data.”
Reinvent training through serious games
“The more powerful technology gets, the more we need to ensure that clinical users can successfully leverage new capabilities. Scaling technology faster and more efficiently calls for new digital tools. The industry of computer games can be an inspiration of how digital tools can reinvent training and accelerate learning for physicians. These virtual technologies can also be a contribution to the Green Deal of the EU, reducing the need for travel and the CO2 footprint. It will also allow to scale innovation globally, democratizing access to adequate health care.”
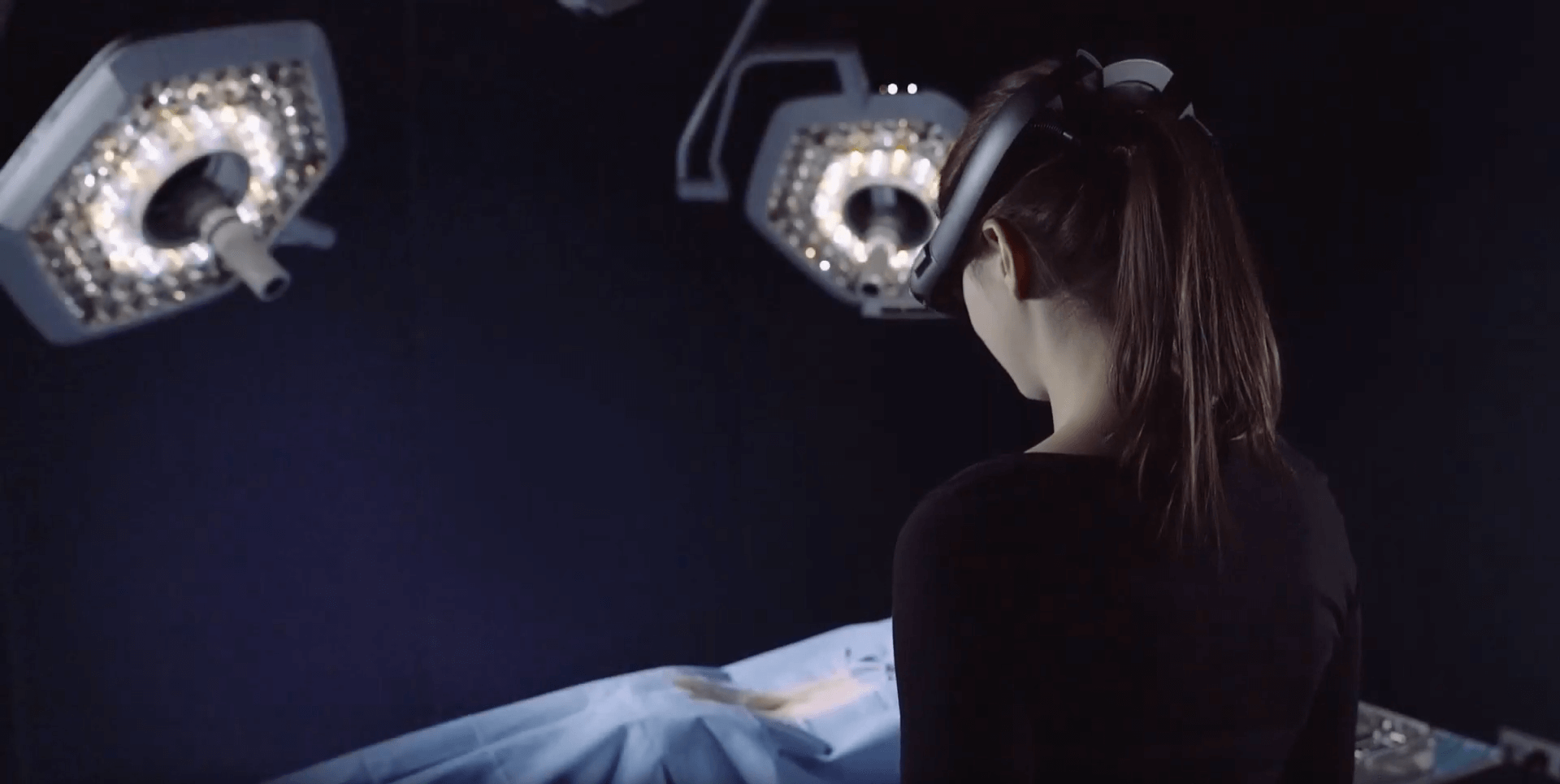
Leverage incremental information using mixed reality
“AI and data-driven innovations will provide us with exponentially growing wealth of information. How can we inject this information into our clinical workflow to maximize its use? Spatial computing, also known as augmented or mixed reality, will be a powerful innovation that will change how we consume and distribute information, merging the digital world with our physical world. AI will detect instruments, events, workflow steps on the fly, and then check the relevant information when and where you need it.”
“The future of healthcare is bright. Never before was the outlook for patients with life-threatening diseases better than right now. Healthcare is one of the few segments in which no American or Chinese digital platform has yet emerged. Together, we can implement a technical solution for the European Health Data Space that can lead the world in innovative capabilities and privacy and, at the same time, promote our values.”