A conversation with Nitesh Paryani, MD Tampa Oncology and Proton Founder and Medical Director
How do physicians decide between radiosurgery, radiotherapy or surgery and what do these approaches mean for patients battling cancer? This video interview with expert radiation oncologist, Nitesh Paryani, MD, answers these questions and more.
Read the transcript below
Joanne: I’m joined today by Dr. Nitesh Paryani, a third-generation radiation oncologist based in Florida. He is the founder and medical director at Tampa Oncology and Proton, a premier cancer treatment group. Dr. Paryani is a highly accomplished expert in the field of radiation oncology, and I’m absolutely thrilled to welcome him here today to give us his insights on the topics of radiosurgery, radiotherapy and cancer in general.
Dr. Paryani, thank you so much for being here. I know your time is limited, so I’m going to go ahead and get started with the first question. When you’re working with a patient, how do you determine if they need radiosurgery, radiotherapy or surgery?
Dr. Paryani: First of all, thank you for having me here today. I really appreciate the opportunity. When we have our radiosurgery program here, we’re lucky that it’s a very multidisciplinary approach. So, I work very closely with our neurosurgeons and our medical oncologists to really come up with a team plan of care for a patient before we implement any sort of intervention. And our neurosurgeons are very involved in our radiosurgery program. They come down to the radiation department and participate in the treatment planning. So, we’re really able to take each patient, and on a case-by-case basis, try to determine what the best course of therapy for them is. For some folks, that means the surgery upfront followed by radiosurgery. For other folks, it’s radiosurgery in lieu of surgery. And, again, I think the benefit of this multidisciplinary approach is there’s not a cookie-cutter way to approach patients, but we really try to identify the individual and unique circumstances for that patient.
Joanne: Well, that actually leads perfectly into my next question, which is a little bit more patient-focused. How can oncology patients inform themselves about their radiation therapy options? For example, if a patient is interested in radiosurgery, what types of questions should they be asking to see if that might be an option for them?
Dr. Paryani: So, I think it’s tough. You know, I always tell folks that it’s kind of easier to research your flat-screen television than it is your own healthcare. You know, we know to go to CNET and other resources for stuff like that, whereas with healthcare, it’s a lot more challenging. I think what patients can do to empower themselves, and I’m a big advocate of patients empowering themselves and really trying to take as much of their own care into their hands as possible, but they really need to be asking questions about the technology that’s being used to treat them. When was the system put in? You know, how many procedures has that doctor or that group of doctors performed? What is their closest competitor? And I always encourage patients to get additional opinions. You know, some cases, obviously, are more urgent than others, but usually, in the radiosurgery world, patients have time to really explore their options and figure out truly what is the best approach for them. And I think that’s a big part of empowering the patient to make the decision that is really going to be, again, uniquely suited for their case.
Joanne: Yeah, it sounds like it becomes more and more precise per patient, and that’s really, really important, I think, in any kind of treatment. So kind of shifting away from the patient focus and moving more towards a general look at this field, can you speak to the standardization of care for radiotherapy and radiosurgery? Are there best practices in place?
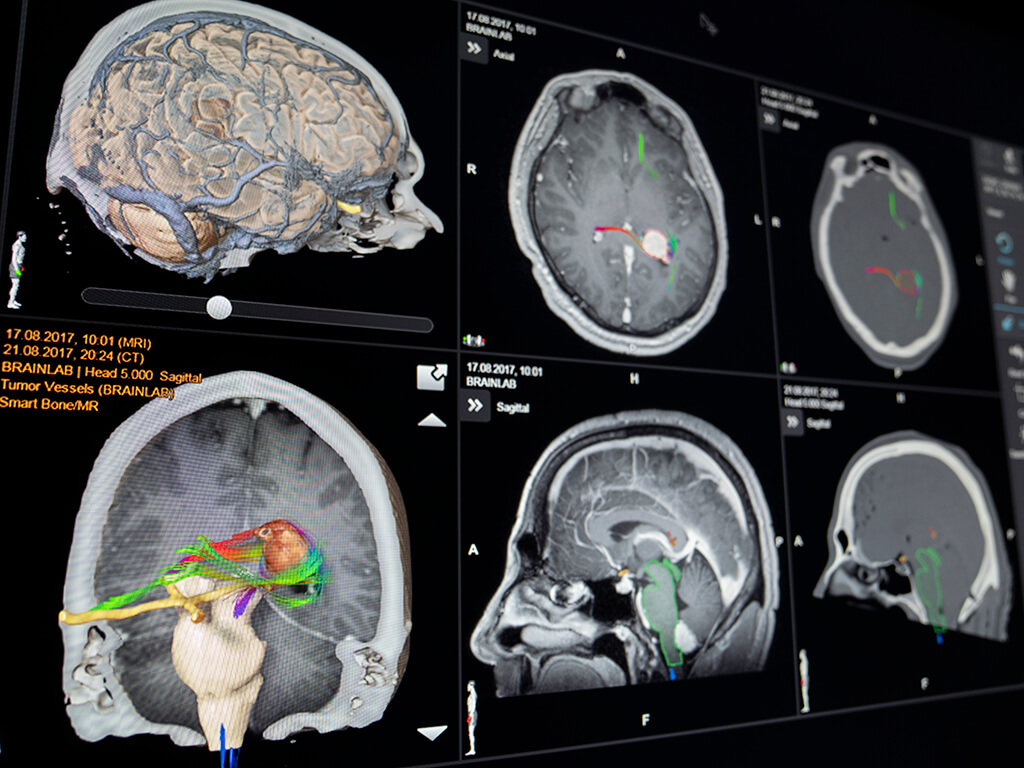
Dr. Paryani: I think there are, and I think it’s tough to say that there’s standardization because there are so many different platforms, so many different approaches, so many different types of tumors that we treat. But I think there are certain best practices that really should be followed when we’re talking about radiosurgery, especially intracranial radiosurgery. You know, I think it’s important that precision and accuracy are at the forefront of the treatment. Imaging, the frequency of imaging, the accuracy of the imaging, all of these things ensure that we are having a reproducible setup for the patient and ensuring that we’re truly targeting where we intend to target, meaning the tumor and, of course, avoiding those critical areas of the brain where radiation can be detrimental and could cause long-term and short-term negative effects. And so I think those are sort of the factors that I push for with patients to say, “Listen, radiosurgery is not typical radiation therapy.” You know, the margin of error in standard radiation therapy is very high. Whereas in radiosurgery, it’s very narrow, and I think having the proper technology and doing the appropriate imaging helps ensure that.
Joanne: That actually fits perfectly with what I wanted to ask next. And you mentioned it, of course, when you think about radiosurgery, you have to think about precision. So my question is, how important is technology then in treatment delivery, and how can technology support in improving patient outcomes?
Dr. Paryani: I think it’s critical. And what I tell patients is… You know, we have a very robust radiosurgery program here, and we treat folks from as far as, you know, several hours away. And I don’t like to have patients travel long distance for treatment that’s not necessary. But what I tell patients about radiosurgery is, “Listen, this is not, again, your typical radiation where we have 20 to 30 treatments, and if one treatment’s slightly off, it’s likely not to impact your long-term outcome.” Oftentimes, these are single-shot, high-dose procedures where accuracy is of the utmost importance because we don’t get another chance. And so I think having that precision is key, having a team that’s comfortable and that does a lot of these is very important, and again, the technology that you’re using behind that. You know, we use the Brainlab system, which I think is extremely useful in that we can image at every angle of treatment. Most radiosurgery programs can’t do that. So we are certain that patients are accurate within millimeters every time we turn that beam on.
Joanne: Well, actually, that brings me to my last question, which is actually about brain cancer. Can you talk about some of the challenges associated with treating cancers of the brain, and how do you overcome those challenges?
Dr. Paryani: Well, I think probably one of the biggest challenges we face with patients can be a wide variety of clinical presentation when they have cancer in the brain. You know, some patients come walking into our clinic. Whereas, others are in the hospital and often intubated, you know, and everything in between. And I think so one of the biggest challenges is really customizing an approach for that patient that they’re going to tolerate, this is going to provide them the benefit that they need. And again, that’s where that multidisciplinary care comes in. You know, oftentimes, some of those patients require a surgical intervention before they can be a good candidate for a radiosurgical procedure, whereas others, radiosurgery is the right answer straight out the bat. So it really kind of is, you know, an important thing to look at. And the challenges we face is, again, every patient’s unique, no two procedures are the same. But I think having the right tools in your toolkit and having the right team on board makes it a lot easier to overcome those challenges.
Joanne: That’s absolutely perfect. Then, those were actually all of my questions for today. So I’m going to thank you so much for your time and for sharing your insights with us. They’re extremely valuable and, of course, beneficial for patients that are battling a cancer diagnosis.
Dr. Paryani: I appreciate your time as well. Thank you for having me.