Webinar
The Benefits of a Digital O.R. in Daily Practice
Description
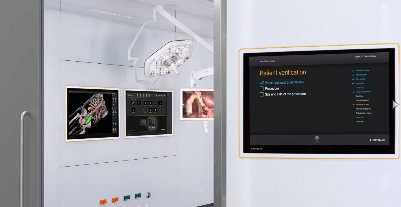
Digitization in hospitals is a topic of growing importance, especially in the O.R. In this session, we will bring together different perspectives from around the world to share the advantages of having a digital O.R. and how it has changed the clinical workflow.
Speaker:

Xavier Escayola, PhD, Bioengineering Department Head
Hospital de Sant Joan de Déu

Albert Busch, MD, Vascular Surgeon
Klinikum rechts der Isar

Daniel Köbsch, O.R. Nurse
Universitätsklinikum Dresden
Moderator:

Matthias Eimer, Senior Manager Digital Health Technologies
See more upcoming webinars
Register now