TL,DR: Revision total hip arthroplasty is performed on patients with an implanted hip joint that is not functioning correctly.
When performed successfully, this surgery can relieve pain, improve mobility and ultimately positively impact quality of life [1]. The article below features the story of an 80-year-old patient that underwent a hip revision surgery and the method and technology that the surgeon, Alexander Greenberg, MD used to perform it successfully.
According to a study [2] published in The Lancet, 3 to 4 percent of people who undergo a hip replacement may require revision surgery within 10 years. Revision surgery is often more complex and less predictable that a primary replacement. As such, specific measures are needed to streamline and improve the procedure to support optimized outcomes for patients.
Read on to learn how Dr. Greenberg and his team at Hadassah Medical Center at Mount Scopus reintroduced mobility into the life of an 80-year-old patient.
Dr. Greenberg is currently an assistant professor of orthopedics at the Hebrew University of Jerusalem and an attending surgeon at the joint replacement and reconstruction unit of the Hadassah Medical Center orthopedic complex.
Dr. Greenberg received his MD from the Hadassah-Hebrew University Medical School in 2009 and completed his residency in orthopedic surgery at Hadassah in 2015. He then went on to a joint replacement fellowship in Cleveland, Ohio, in 2016, after which he returned to Hadassah as an attending surgeon. In 2019 he completed another fellowship year in complex joint reconstruction at the Hospital for Special Surgery in New York.
Problem
In 2022, 80-year-old patient “Mr. A” visited the Hadassah Medical Center at Mount Scopus due to pain in his operated hip. Mr. A had suffered a hip fracture in 2021 and was operated elsewhere. Unfortunately, he still found walking very difficult and had to use a motorized scooter.
During the initial physical examination, Dr. Greenberg found that the patient could hardly bear weight on the operated leg, had a tender range of motion of the hip and shortening of the right leg.
The surgical wound from the initial hip replacement surgery was clean, dry and intact. A pelvis X-Ray showed a right cemented unipolar non-modular (monoblock) hemiarthroplasty with minimal cement in the distal part of the implant. The X-Ray indicated that the right leg was shortened as well. Bloodwork was performed and confirmed a normal CBC, ESR and CRP.
Method
Dr. Greenberg and his team performed a hip aspiration that yielded no intra-articular fluid directly followed by a lidocaine test. This immediately resulted in marked pain reduction and an improvement in Mr. A’s walking ability. A bone scan was performed that demonstrated diffuse uptake around the femoral stem. A diagnosis of aseptic loosening was made and the patient was referred for a hip revision.
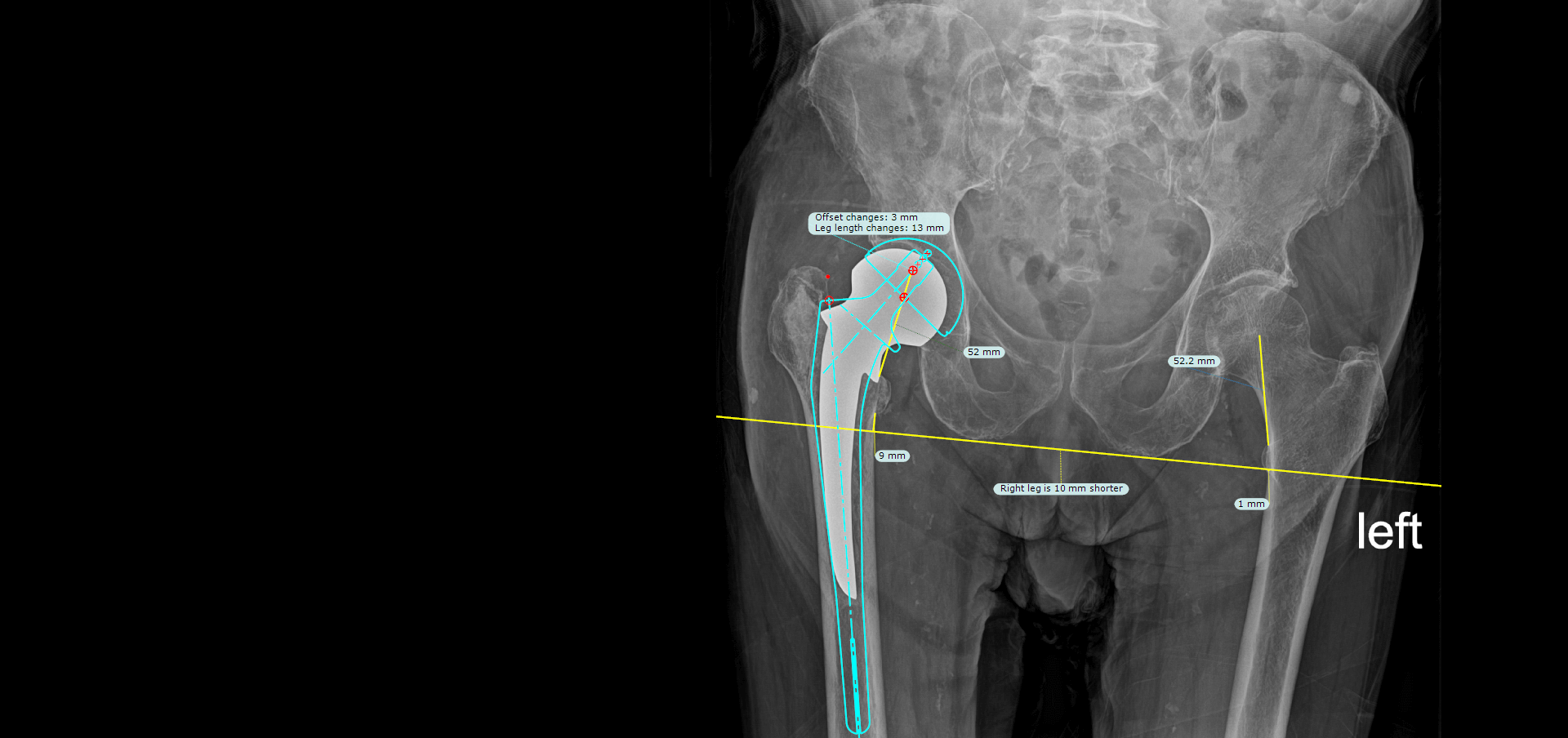
The revision surgery was planned using the Brainlab software TraumaCad. The objective was to implant an acetabular cup and revise the femoral component to restore the patient’s leg length and offset, while ensuring stability of the femoral stem.
During the surgery, there were no signs of infection. Routine cultures were sent to the lab and the femoral stem was grossly loose. The cement mantle was carefully extracted using revision osteotomes. A primary hemispherical cup was implanted in the acetabulum and augmented with two screws. A fully hydroxy-apatite coated revision stem was implanted in the femur as per the pre-operative TraumaCad plan to restore the patient’s hip biomechanics.
Outcome
Six weeks after the surgery was performed, Mr. A reported a marked improvement in pain. He was also able to walk using only one cane.
The surgical wound was clean and dry and intact, and the hip range of motion remained minimally tender. Pelvis X-Rays showed restored leg length and hip offset with well-positioned implants and no interval change compared to immediate post-operative X-Rays. Cultures from the surgery were also negative.
Conclusion
“To us, this case highlights the importance of a thorough preoperative work-up, diligent pre-planning and careful execution of the operative plan. We were happy we could help this Mr. A regain his mobility and independence,” commented Dr. Greenberg.
1. Cleveland Clinic. Hip Revision
2. Deere K, Whitehouse M, Kuntsor S, Sayers A, Mason J, Blom A. How long do revised and multiply revised hip replacements last? A retrospective observational study of the National Joint Registry. https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(22)00097-2/fulltext. Published July 2022.