Webinar
Benefits of navigation and intraoperative imaging in Cranio-Maxillofacial Surgery – a clinical case review
Feb 09, 2021
Description
Brainlab invites you to join our live webinar, “Benefits of navigation and intraoperative imaging in Cranio-Maxillofacial Surgery – a clinical case review”, on February 9, 2021 at 4:00 PM CET presented by Prof. Julio Acero, MD, DMD, PhD, President of the European Association for Cranio-Maxillo-Facial Surgery, Head of the Department of Oral and Maxillofacial Surgery of the Ramón y Cajal University and the Puerta de Hierro University Hospitals in Madrid, Spain, and Professor of Surgery at the Alcala University of Madrid.
In this webinar you will:
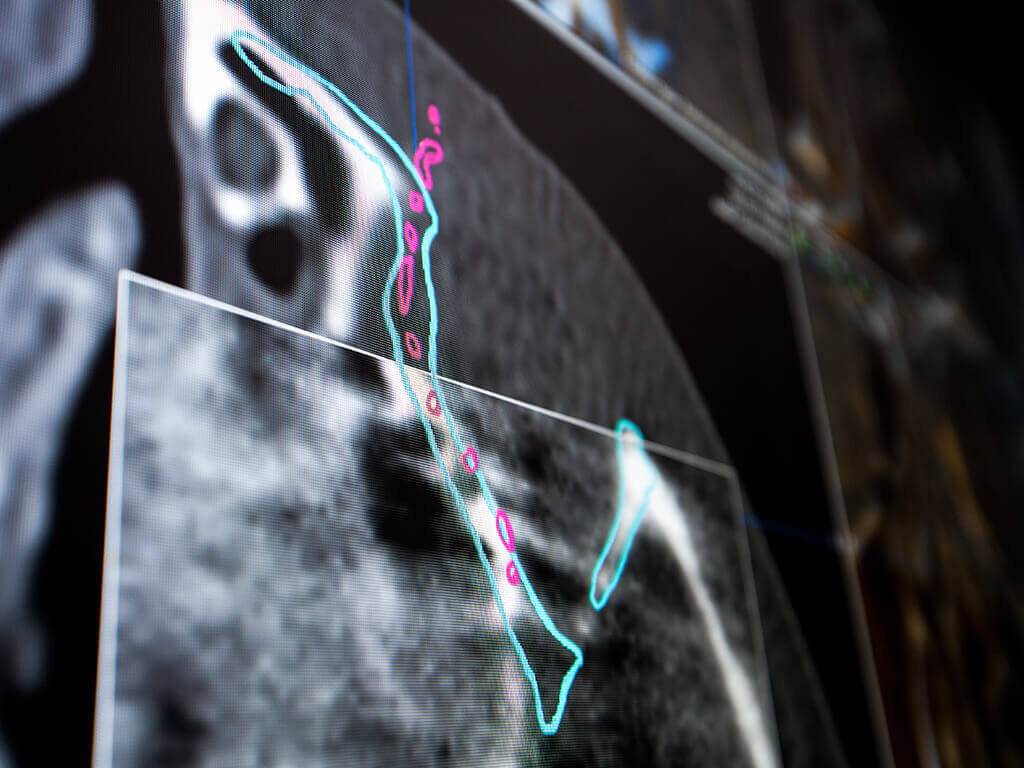
Understand the benefits of virtual planning combined with navigation assisted surgery in craniomaxillofacial surgery
Be familiarized with the workflow concerning the use of navigation and intraoperative imaging
Learn how intraoperative imaging can help to improve outcomes in complex craniomaxillofacial procedures
We look forward to meeting you online!
Language | English
In case you can not join the webinar, it will be recorded and shared afterward.
Participation is free of charge.
The views, information and opinions expressed within this presentation are from the speakers and do not necessarily represent those of Brainlab.

Prof. Julio Acero, MD, DMD, PhD
Ramón y Cajal University and Puerta de Hierro University Hospitals, Madrid, Spain
