It’s a sunny spring morning in Schwäbisch Hall, a town of 40,000 in southern Germany, located between Stuttgart and Nuremberg. Dr. Huber-Wagner is Chief of Trauma Surgery, Spine Surgery and Geriatric Trauma Care at Diak Klinikum, the county hospital for Schwäbisch Hall. Today, he’s operating alongside senior consultant Thorsten Möhlig and his team on a patient in his early 70s. A metastasis has almost completely destroyed the patient’s first thoracic vertebra. The goal of the operation is to stabilize the spine. “If we don’t intervene, there’s a real risk of spinal collapse—which could result in paralysis,” Dr. Huber-Wagner explains.
He had planned the procedure the day before, using a computer. That’s important to him—having the patient’s anatomy, with all its unique details, already in his mind when he wakes up in the morning. “You’re just better prepared when you step up to the operating table.”
He plans to place nine screws into the healthy vertebrae above and below the tumor, then connect them using a titanium rod to stabilize the entire section. He’ll also take a tissue sample from the tumor for testing, which will help guide the next steps in cancer treatment.
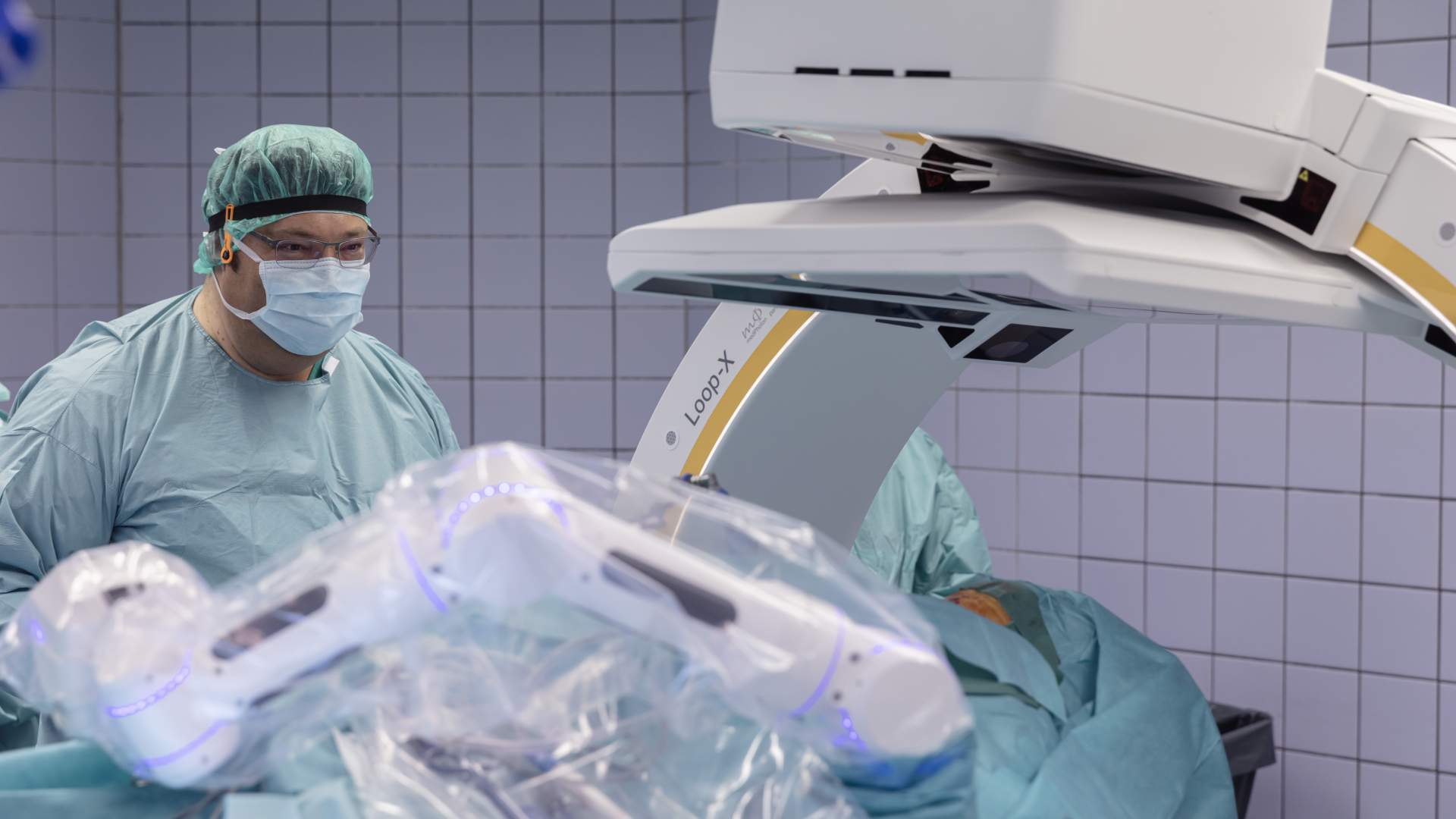
For each screw, Dr. Huber-Wagner has defined the entry point, angle, depth and diameter—based on CT images taken a few days earlier. To ensure the screws are placed exactly as planned, he’s been using the Brainlab Robotic Suite since 2022. The system was made available to the hospital thanks to a private donation from the Gerhard and Ilse Schick Foundation, which supports innovative projects, particularly in the region around Schwäbisch Hall.
The innovative project enhancing Dr. Huber-Wagner’s O.R. today includes a 3D imaging robot, a robotic arm and a high-precision navigation system. It may sound a bit like Google Maps—and in some ways, it works like it too. On the monitor, the surgical team can follow exactly whether they’re placing the screw on the pre-defined path through the vertebra.
Compared to standard x-rays, intraoperative 3D CT scans offer two key advantages: they can capture much larger areas, such as the entire pelvis, and the high-resolution images can be tailored to each individual patient.
“In the cervical spine, for example, the shoulders often block the view of the affected vertebrae—on an x-ray, you can hardly see anything at all,” Huber-Wagner explains. “Thanks to Loop-X, we can capture much more detail in the area that matters—while also exposing the patient, and ourselves, to less radiation.”
So how would this kind of operation go without high-tech navigation, advanced 3D imaging and robotics? “We would have planned the procedure completely differently—and, most importantly, used different and shorter screws,” Huber-Wagner explains.
Shorter screws mean shallower drilling and more distance from critical structures, but also less stability. “If each screw doesn’t hold as much, you have to place more of them—and include more healthy vertebrae in the operation.”
Would it even be possible to place these stronger, so-called pedicle screws without navigation? “Of course, with a lot of experience, you can do it,” he says. “But I personally wouldn’t want to undergo cervical spine surgery without navigation.”
He laughs briefly, then turns serious. “You know—surgeons don’t get a second chance.”
“Even if you’ve performed a procedure successfully a thousand times—a mistake on the thousand-and-first will still count against you. You can’t make up for it with your past ‘heroics.’”

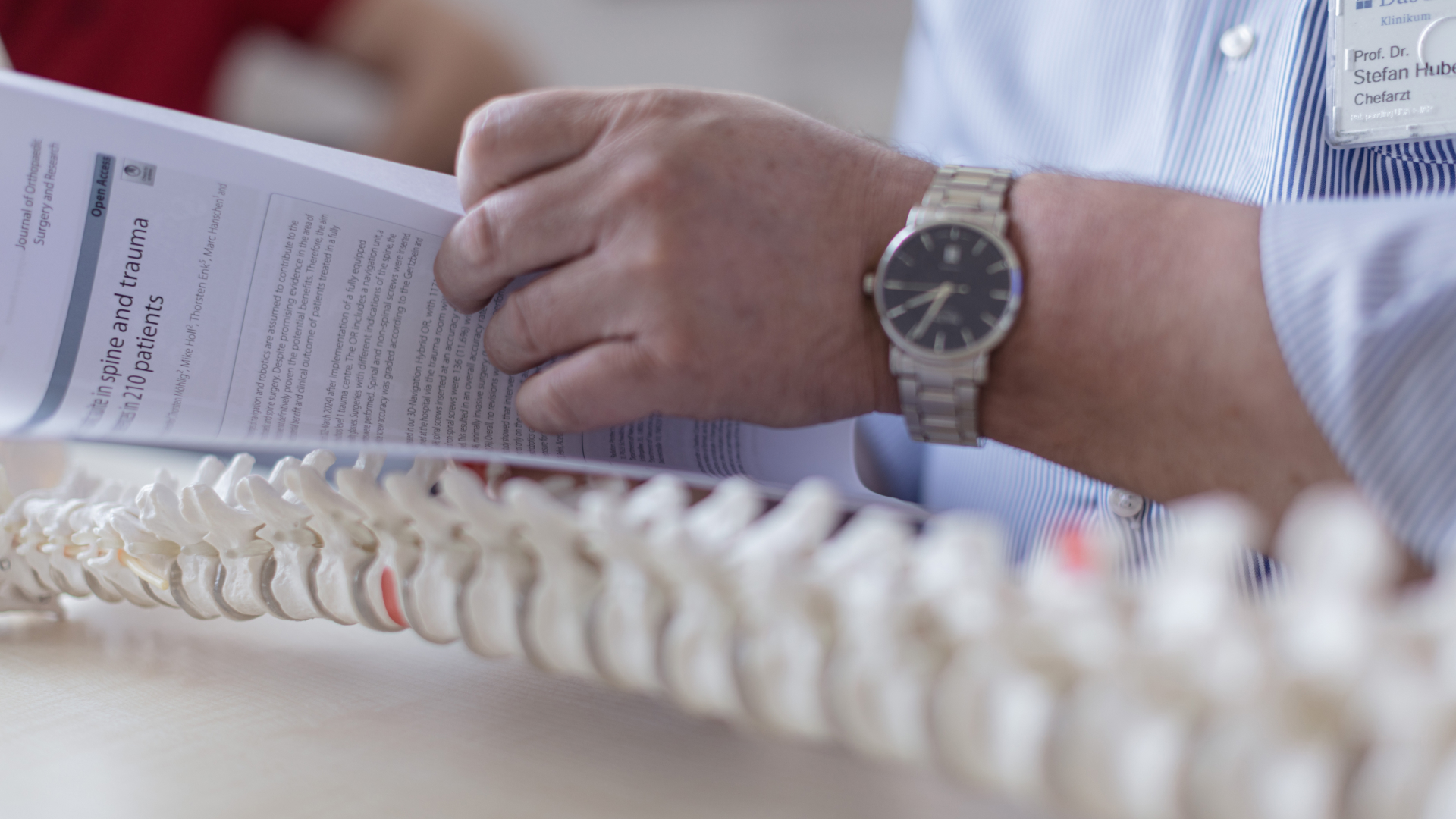
That’s likely why it was so important to Dr. Huber-Wagner from the beginning that the Brainlab Robotic Suite wouldn’t just be a flashy tool in the O.R. to make the work easier for him and his team—but that it would also deliver hard data on whether the technology really improves patient safety.
Of the roughly 1,200 screws placed in those surgeries, 98.8 percent ended up exactly where they were supposed to. Not a single one had to be repositioned in a second surgery due to critical misplacement.
“That’s pretty damn good,” says Dr. Huber-Wagner. For comparison: with conventional screw placement— that is, without navigation or robotic assistance—the global average misplacement rate is estimated at around 15 percent. Soon, once they’ve reached the 2,000th-screw mark, he plans to conduct another analysis. “But from what I’m seeing so far, I think we’ll be able to confirm the findings from the first study.”
The experience that he and his team have gathered across all these procedures has also made him a sought-after point of contact for colleagues from around the world. “About every two weeks, someone comes to visit,” he says. “It’s a good, collegial exchange—and I think people do pick up a thing or two from us.”
The questions tend to focus less on the technology itself and more on practical details: how to position the patient, where best to place the reference array, how to handle unusual anatomy, and so on.
“You can’t just want a system like this—you have to actually use it. And you have to stay open and curious. That’s the only way to really unlock its full potential.”

At Diak Klinikum in Schwäbisch Hall, it’s clear they’re fully committed to working with the Robotic Suite.
“One of our most senior O.R. nurses was a bit skeptical at first,” Dr. Huber-Wagner says, laughing. “Now he’s almost disappointed when we do a procedure without navigation.” Good thing surgery number 335 with navigation is scheduled for the next day.