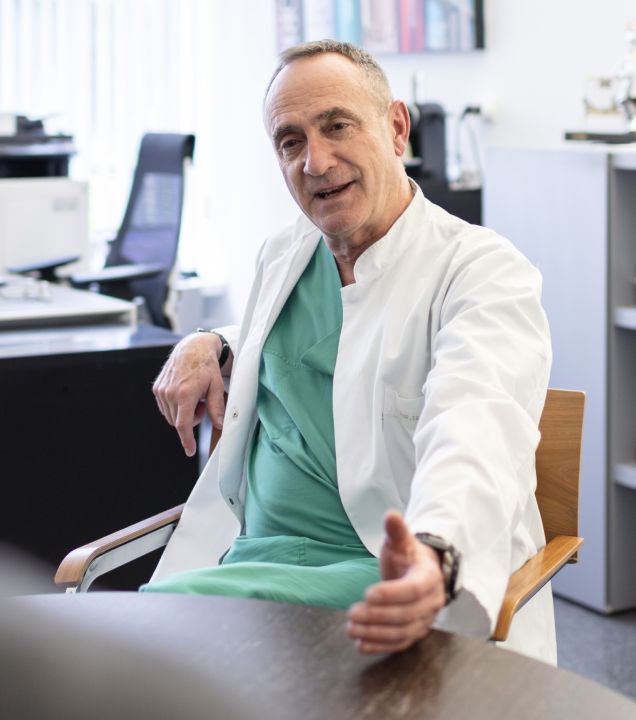
Robots in the operating room—it still sounds a bit futuristic. But what really matters when it comes to making them useful for doctors and patients? Professor Bernhard Meyer, MD, Director of Neurosurgery at the Technical University of Munich, and Nils Ehrke, President EMEA at Brainlab, explain why robotics in the O.R. isn’t an end in and of itself, the value robotics can bring, and what high-performance surgery has in common with professional sports.
Professor Meyer, how much of robotics is actually part of everyday surgical practice today and how much is just hype?
Professor Meyer: It’s important to make a distinction. When we hear "robotics," it often sounds like something out of the future—machines performing surgery on their own. But we’re still many years away from that. What’s currently referred to as robotics in the O.R. is usually a form of semi-automated navigation. These are more like assistance systems that can support surgical workflows, which is a pretty good start, but of course, it’s not the same as a robot performing surgery.
What do you expect from technology in the operating room?
Professor Meyer: My goal is simple: I want to operate. Efficiently, safely and without distractions. Everything outside of that—navigation, imaging, preparation—needs to support me, not slow me down. That’s why new technologies don’t just need to be better; they have to be faster, or at least not slower than our existing methods. Otherwise, we won’t use them. I don’t want to be held back by technology. And I want to be able to think. Technology should create space for that—not take it away.

Professor Bernhard Meyer, MD, is President of the German Spine Society and has led the Department of Neurosurgery at Klinikum rechts der Isar, Technical University of Munich, since 2006—one of the most respected neurosurgical centers in Europe. He is recognized as a leading expert in spine and skull base surgery, has helped shape several international medical societies, and is known for driving innovation with a pragmatic approach.
Mr. Ehrke, Professor Meyer just mentioned that robotics can support surgical workflows—what does that actually mean?
Nils Ehrke: One example is a robotic arm that can move to a planned position with millimeter precision and then guide surgical instruments with the same accuracy. Our goal is to support surgeons in a very targeted way—but that only works when teams treat robotics as part of a well-designed overall process. It only creates value when paired with navigation—the system that tells the robot where it needs to go in the first place.
Robotics and navigation work as a technical unit. But they only reach their full potential when surgical teams embed them in a workflow tailored to each patient. The anatomy, the planning, the procedures in the O.R.—everything needs to work together.
A lot of hospitals invest in robotics to appear cutting-edge. But if they don’t treat clinical workflow as an integrated part of both the technology and the treatment, even the most advanced robot won’t help. Our experience shows that the real value comes from the interplay of precise imaging, careful planning, surgical navigation and a clinical workflow built around the technology. Robotics can be a powerful addition to that process—but it should never be the starting point.
So what does the optimal workflow look like—and why does it have such a strong impact on the success of robotics?
Professor Meyer: To understand that, you first have to consider how a navigation system actually works. It aligns a planning image—such as a CT scan—with the actual patient lying in front of you. Once the registration is complete, the patient—especially the spine—has to stay completely still.
In the past, when placing screws, we used tools called awls—rigid guiding instruments that required a lot of pressure on the spine. That pressure could cause slight movement, which would throw off the navigation system—and of course, the robot along with it.
So we adjusted our workflow in the operating room. Today, we start by pre-drilling with a high-speed drill—you can picture it like a cordless drill from a hardware store. It works with almost no pressure, so the spine stays stable. Then we insert a thin wire, called a Kirschner wire, into the hole. That wire serves as a guide, helping us place the screw precisely along the planned path. This reduces potential sources of error. And in the end, I have a method that saves me time and increases precision.
Nils Ehrke: I actually experienced this workflow in detail for the first time right here at Professor Meyer’s clinic—and I immediately saw that we should be recommending it to our customers, even before they start thinking about buying a robot. Understanding the principles of surgical navigation—and building an optimized workflow around them—is the foundation for using robotics. Only when all of those components work seamlessly together can robotics reach its full potential, for both the surgical teams’ and the patients’ benefit. You could compare it to the concept of marginal gains in professional sports: lots of small improvements—in imaging, planning, registration, or clinical workflow—add up to a meaningful increase in overall quality. Robotics isn’t the solution on its own, but part of a system that becomes stronger as a whole.
How do patients benefit?
Professor Meyer: First of all, we can now operate on people who, 15 years ago, would have been considered “inoperable”—even patients in their 80s and older. Because we know: if we do it right, we can give them back a lot of quality of life. The benefits are significant. We’re constantly pushing the boundaries of what’s possible, with care and good judgment. Today, it’s standard to use navigation in spine surgery. Fifteen years ago, it was still considered unusual. Now, we place screws with navigation—quickly, safely and minimally invasively.
And the fact that we’ve developed a workflow that saves us time benefits patients, too. First, it means we can treat more people. Second, especially with older patients, every minute we can spare them from staying under anesthesia counts.
Experience new surgical possibilities with Loop-X
As a highly respected neurosurgeon—which you undoubtedly are—do you ever worry that navigation and robotics might one day make surgery so simple that anyone could do what only you could before?
Professor Meyer (laughing): That should always be the goal—that today, my colleagues can perform procedures that, a few years ago, would have required some kind of top expert. That’s what we call progress.
And by the way, I don’t think these technologies make everyday work easier for truly skilled surgeons—quite the opposite. The more experienced you are, the more complex cases you take on. That raises the demands on the treatment and the technology. Because the better we get, the more we push the limits of what’s possible, step by step. Responsibility grows with expertise. And in the end, what really counts is still the same: experience, judgment and the ability to make the right call under pressure.
Is there a core mindset that every good surgeon needs to have?
Professor Meyer: Absolutely. You can’t hesitate. In the O.R., you’re making decisions constantly—sometimes every second. If you start second-guessing, it’s already too late. A surgeon needs to be focused, decisive and honest with themselves. I’m not a fan of overinflated egos in the operating room. It’s not about one “star surgeon”—it’s about consistent, reproducible quality.
The real question is: can you enable others to make decisions just as good as the ones you would make yourself? To me, that’s true excellence.


Back to robotics: What would you recommend to hospitals considering an investment in this technology?
Nils Ehrke: First, optimize your workflow: navigation, imaging, surgical routines. And once that’s in place, a robot can complement the process. But not the other way around. If you buy the robot first and then try to build everything else around it, it’s going to be much harder to get the most out of your investment.
Professor Meyer: I completely agree. I’m always in favor of innovation. But I also believe in honest technology and realistic promises. I find robotics incredibly exciting—but if someone acts like it magically makes everything better, I get skeptical. A strong clinical workflow without a robot will always bring more value than a robot without a strong clinical workflow.
“But we have to stay vigilant. Technology should never be an end in itself. It should strengthen the team—not replace it.”
One last question: Looking ahead, how do you see the future of surgical robotics?
Professor Meyer: I think in five to ten years, we’ll start to see the first systems capable of truly autonomous—or at least semi-autonomous—functions, especially once sensor technology and AI are properly integrated. The key will be haptics: robots that can sense whether they’re working through bone or soft tissue will change a lot. But we have to stay vigilant. Technology should never be an end in itself. It should strengthen the team—not replace it.



