网络研讨会
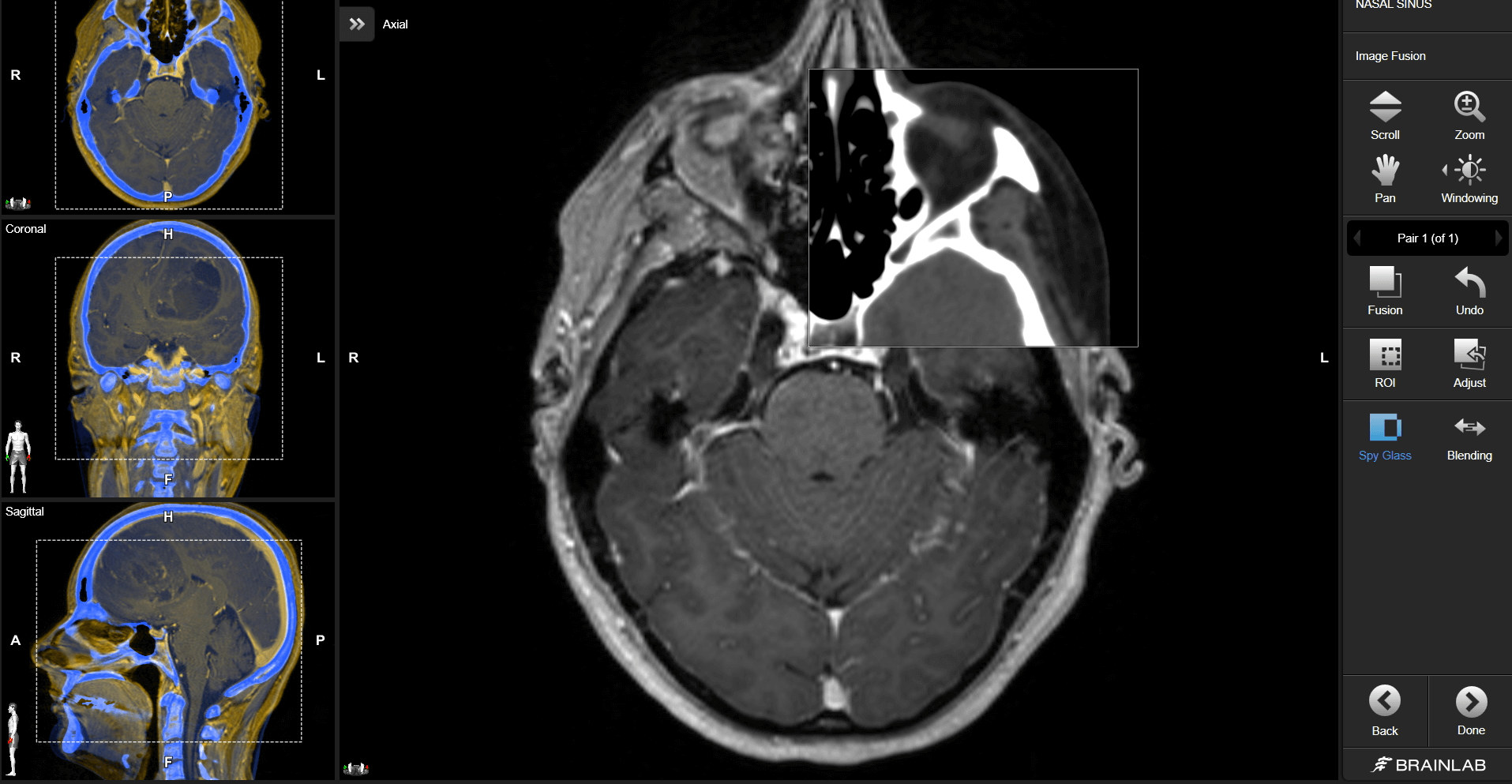
Complex Case Discussion Focusing on Navigation and Image Fusion in Sinonasal Tumors
Mar 10, 2021
描述
Brainlab invites you to join a live webinar, “Complex Case Discussion Focusing on Navigation and Image Fusion in Sinonasal Tumors”. Taking place on March 10, 2021 at 4:00 PM CET, this webinar will be presented by Frank Haubner, MD, Senior Physician, Department of Otolaryngology, University Hospital Munich, Germany.
We look forward to meeting you online!
Language | English
In case you can’t join the webinar, it will be recorded and shared afterward.
Participation is free of charge.
The views, information and opinions expressed during this presentation are the speaker’s own and do not necessarily represent those of Brainlab.
演讲人

Priv. Doz. Dr. med. Frank Haubner, Senior Physician, Department of Otolaryngology
University Hospital Munich, Germany, Munich, Germany
主持人

Jana Guggenberger, Director Product Management & Marketing Spinal/CMF Planning/Navigation
查看更多即将开展的网络研讨会
马上注册