Dr. Greenberg is currently an assistant professor of orthopedics at the Hebrew University of Jerusalem and an attending surgeon at the joint replacement and reconstruction unit of the Hadassah Medical Center orthopedic complex.
Dr. Greenberg received his MD from the Hadassah-Hebrew University Medical School in 2009 and completed his residency in orthopedic surgery at Hadassah in 2015. He then went on to a joint replacement fellowship in Cleveland, Ohio, in 2016, after which he returned to Hadassah as an attending surgeon. In 2019 he completed another fellowship year in complex joint reconstruction at the Hospital for Special Surgery in New York.
Case Summary
Background
A 36-year-old female patient came to the clinic in 2022 with bilateral hip pain, a limp and lower back pain.
During a physical examination, she was found to have a bilateral Trendelenburg gait. The doctors also noticed a considerable lumbar hyperlordosis, and upon further examination, observed a positive Thomas test and a limited bilateral hip range of motion.
Patient History
This patient underwent hip surgery as a child but was unable to provide additional information about the procedure.
However, the doctors had access to an X-Ray from 2014 where they were able to see she had an advanced hip disease on both sides as well as a type of dysplastic pelvis.
In 2014, the patient decided to wait for surgery as the pain was relatively low and manageable. The patient initiated nonsurgical therapy, which she continued for several years.
Nonetheless, in 2022, she arrived at the clinic with severe arthritic changes on both her hips and a pelvis that was even more rotated compared to the X-Ray from 2014.
Treatment Method
Based on the physical examination, X-Rays and patient history, the team began planning an arthroplasty.
The patient requested to have the first surgery on her left hip because that was more painful at the time. However, the standard approach for this type of procedure—using a regular tapered wedge stem—would not work due to the patient’s unique anatomy.
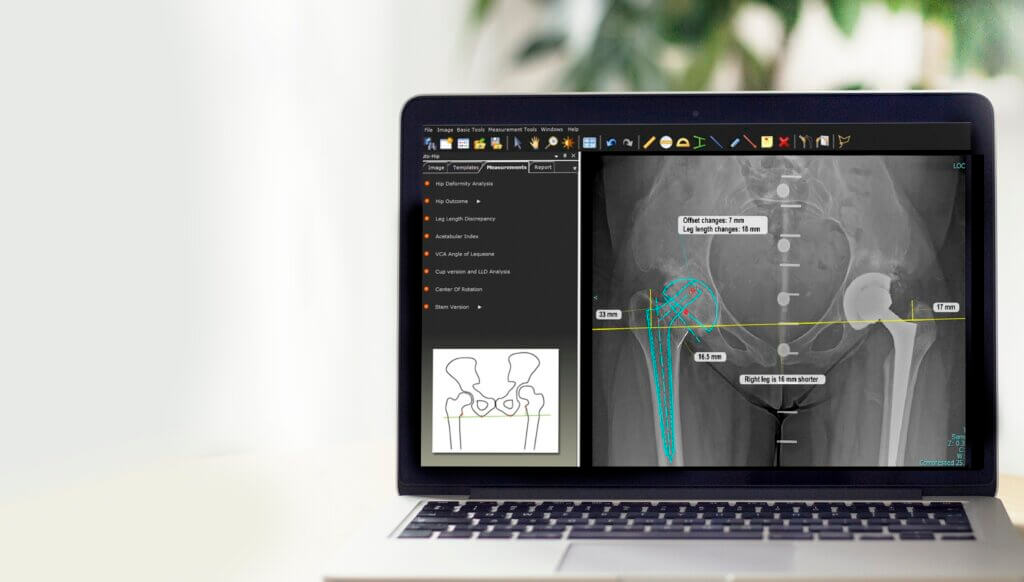
To identify and plan a viable solution, the surgical team used TraumaCad. This software allows orthopedic surgeons to simulate their expected results prior to procedures to create smooth surgical workflows from start to finish.
In this case, TraumaCad software enabled the surgical team to simulate various options and stem lengths which ultimately kept the procedure as close to a standard arthroplasty as possible.
Outcome
Six weeks after the first surgery on the left hip, the patient reported that she had experienced a marked reduction in pain. Her pelvis was also beginning to regain its original orientation.
Following her report, the patient requested surgery on her right hip, which again, using a similar patient-specific approach and TraumaCad technology, resulted in a positive outcome.
Six weeks after the right hip replacement, the patient was able to walk with a very mild limp and an almost completely straight back. Her lumbar hyperlordosis was cured as well.
Conclusion
When working with patients that have a very unique anatomy, surgical teams need to think outside the box. One size and approach does not fit all, even if that may work for about 90% of patients.
“When you go through a meticulous preoperative planning process, you can restore patient anatomy and function much better. It gives you a lot of confidence that you’re going into surgery knowing that you have both a plan and a backup plan. Once you execute that plan in surgery, it makes you feel much more confident and gives good results to your patients.” – Dr. Greenberg
Want to learn more about TraumaCad? Click here for details: https://www.brainlab.com/surgery-products/orthopedic-surgery-products/orthopedic-templating-software/